Hamid Esmaeilpour*
General Surgeon, Dar Al Kamal Hospital, Sharjah, U.A.E
*Corresponding author: Hamid Esmaeilpour, General Surgeon, Dar Al Kamal Hospital, Sharjah, U.A.E.
Citation: Esmaeilpour H (2025) Laparoscopic Removal of the Uterus: Procedure, Benefits and Postoperative Care. Glob J Surg Surgical Res 1(1): 43-55.
Received Date: 25 April 2025; Accepted Date: 20 May 2025; Published Date: 23 May 2025
Abstract
Laparoscopic removal of the uterus is one of the minimally invasive methods for hysterectomy, which has several advantages compared to open surgery, such as reduced bleeding, faster recovery, less pain, and reduced length of hospitalization. This procedure, which is performed using a laparoscopic camera and special instruments through small incisions in the abdomen, has gained popularity in recent years due to the reduction of postoperative complications, reduction of hospital costs, and increase in the quality of life of patients have become more important. According to the World Health Organization (WHO), more than 1.2 million hysterectomys are performed annually in the United States, more than 40% of which are laparoscopically. Studies show that the success rate of this procedure is more than 98%, and the rate of complications is less than half compared to open surgery. Also, the average length of hospital stay for patients undergoing laparoscopic surgery is 1.5 days, while This number reaches more than 4 days in open surgery. In addition, the time to return to daily activities in laparoscopy is almost twice as fast as in open surgery. However, the procedure requires advanced equipment and skilled surgeons and is not suitable for some patients with severe obesity or pelvic adhesions. Due to the increasing demand for minimally invasive procedures, it is predicted that by 2030, more than 60% of hysterectomy surgeries will be performed laparoscopically. Overall, laparoscopic hysterectomy is an effective, safe, and cost-effective procedure that can be considered as a viable alternative to open surgeries in many cases.
Keywords: Bleeding reduction; Hysterectomy; Laparoscopy; Less pain; Minimally invasive surgery; Open surgery; Recovery time
Introduction
In recent decades, medical advances and new surgical technologies have led to the introduction of minimally invasive methods such as laparoscopy as an effective alternative to open surgeries. One of the most important applications of this technique is laparoscopic hysterectomy or laparoscopic hysterectomy, which is used to treat diseases such as uterine fibroids, endometriosis, abnormal bleeding, uterine and ovarian cancers, and uterine prolapse. While in the past, surgery Again, due to better access to internal organs, laparoscopy has become the preferred option for many patients and surgeons today due to reduced bleeding, less pain, reduced recovery time, and faster recovery. The procedure is performed through several small incisions in the abdomen, in which a laparoscopic camera and special surgical instruments are inserted into the body and the uterus is removed without the need for a large incision. According to reports published by the World Health Organization (WHO), millions of hysterectomy cases are performed annually around the world, of which more than 40% are performed laparoscopically in developed countries. Studies Clinical studies show that the success rate of laparoscopy is more than 98 percent, and the rate of complications is significantly lower than that of traditional surgeries. In addition, the period of hospitalization of patients is reduced and the time to return to daily activities is faster. However, this procedure is not suitable for all patients and presents some challenges such as the need for advanced equipment, higher initial cost, and the need for more experienced surgeons. Due to the increasing growth of this technique, it is expected that in the coming years, laparoscopy will replace more invasive methods as the gold standard in hysterectomy surgery. In this article, we will explore the process of performing laparoscopy, advantages, disadvantages, related statistics And we will discuss the future of this surgical procedure.
Research Background
Pedrosa et al.'s article explores the difficulties associated with laparoscopic hysterectomy and surgical strategies to overcome these challenges. The main challenges include pelvic adhesions, anatomical changes, and intraoperative bleeding. The authors recommend various techniques to manage these problems, including the use of advanced instruments and methods to protect vital structures such as ureters. The article emphasizes the importance of proper education and learning curves for surgeons It emphasizes and provides strategies for choosing the right patient. The authors conclude that despite the technical challenges, laparoscopic hysterectomy can be performed with high safety and efficacy, provided that surgeons are well-trained and use appropriate strategies to manage potential problems. [1]. Kaposi et al.'s article investigates urological complications after laparoscopic hysterectomy in gynecologic oncology patients. This study investigates the prevalence, risk factors, and methods of managing urinary tract injuries, especially ureteral and bladder injuries. Patients with gynecological cancers are at higher risk for these complications due to tumor spread and anatomical changes. The authors discuss methods for prevention, early diagnosis, and treatment of these complications. discuss and emphasize the importance of accurate identification of anatomy, the use of standard surgical techniques, and regular follow-up of patients. By adopting appropriate surgical methods and postoperative care, urological complications can be minimized [2].
Merv et al.'s article explores Laparoendoscopic Single-Site Hysterectomy (LESS). The benefits of this procedure include better cosmetic results, less postoperative pain, and a faster return to daily activities. The authors describe technical details, including specific instruments required, insertion techniques, and technical challenges such as maneuvering limitations and instrument interference. It also examines the complications, contraindications, and learning curve of the procedure for surgeons. LESS can be a safe and effective option for selected patients, but it requires advanced laparoscopic skills and specific training. The article concludes with suggestions for the successful implementation of this procedure in surgical centers [3]. Maduki-Lavo et al.'s article examines the long-term risks of hysterectomy for benign cases. The authors have identified evidence of an increased risk of cardiovascular disease, osteoporosis, mental disorders, and pelvic floor problems after hysterectomy. The article points to the hormonal and metabolic effects of uterine resection, even in cases where the ovaries are preserved. The authors stress the importance of carefully examining indications for hysterectomy and considering conservative treatment optionsThey emphasize and advise that patients should be aware of potential long-term risks. Although hysterectomy is effective for many benign conditions, it should be considered as a last resort and long-term follow-up is essential for patients [4].
The paper by Haddad et al. compares laparoscopic and laparotomy procedures in radical hysterectomy surgery for endometrial cancer. Laparoscopy has significant benefits such as less bleeding, less postoperative pain, faster return to daily activities, and smaller scars. The technical challenges of laparoscopy include a longer learning curve, longer operating time, and equipment costs. In terms of oncological outcomes, laparoscopy can have the same survival results with laparotomy Be. Laparoscopy can be a safe and effective option for selected patients with endometrial cancer, but decisions should be made based on the patient's individual circumstances, stage of the disease, and the surgeon's experience. [5] The article by Madovani et al. deals with the prediction of major complications in patients undergoing laparoscopic and open hysterectomy for benign cases. The authors have identified predictive factors for complications based on clinical and demographic data such as age, body mass index, comorbidities, uterine size, and previous surgical history. There are some risk factors common to surgical procedures, but others are specific to each procedure. Data Prediction ModelIndependently validated and performed well. This model can help surgeons select the right patients for each surgical procedure, better prepare for high-risk cases, and improve the informed consent process. The use of predictive models can lead to a reduction in complications and improved outcomes [6].
The article by Joanna et al. provides a systematic overview of surgical outcomes in laparoscopic hysterectomy, robot-assisted hysterectomy, and laparoscopic assisted vaginal hysterectomy for uterine and cervical cancers. All three procedures have acceptable results, but they have their own advantages and disadvantages. Robot-assisted hysterectomy has advantages such as greater precision and less surgeon fatigue, but it also entails higher costs. Article on Growing Usage It mentions minimally invasive procedures in gynecologic oncological surgeries. Choosing the right procedure should be based on the patient's characteristics, the stage of the cancer, the surgeon's experience, and available resources. More research is needed to directly compare these methods with the design of more robust studies [7].
The article by Georgie et al. deals with the prevention and treatment of intraoperative complications in laparoscopic gynecologic surgeries. The authors address complications such as vascular, intestinal, urinary tract injuries, and heat-energy-related complications. Preventive strategies are described including proper preoperative preparation, safe entry techniques, accurate identification of anatomical structures, and the correct use of energy instruments. Methods for early diagnosis and management of complications when they occur with Details are described. The article emphasizes the importance of continuous education, simulation, and learning from past experiences to reduce the risk of complications. Although complications are inevitable in laparoscopic surgery, proper preparation and rapid response can significantly reduce their outcomes [8].
Sutton's article delves into the history of hysterectomy from ancient times to the modern era. The author describes the earliest recorded reports of uterine resection, early techniques, and the high mortality rates associated with it. Important milestones include the first successful abdominal hysterectomy in the 19th century, the development of vaginal hysterectomy, and important advances in anesthesia, infection control, and surgical techniques that led to a significant reduction in mortality. Evolution Indications for hysterectomy are being investigated from use only for life-threatening conditions to wider application for benign diseases. The article concludes with a look at contemporary advances such as laparoscopic hysterectomy and robotic approaches. (Sutton, ## 150-point summaries of articles with in-text references Pedrosa et al.'s article explores the difficulties associated with laparoscopic hysterectomy and surgical strategies to overcome these challenges. The main challenges include pelvic adhesions, anatomical changes, and intraoperative bleeding. The authors recommend various techniques to manage these problems, including the use of advanced instruments and methods to protect vital structures such as ureters. The article emphasizes the importance of proper education and learning curves for surgeons It emphasizes and provides strategies for choosing the right patient. The authors conclude that despite the technical challenges, laparoscopic hysterectomy can be performed with high safety and efficacy, provided that surgeons are well-trained and use appropriate strategies to manage potential problems [1].
Kaposi et al.'s article investigates urological complications after laparoscopic hysterectomy in gynecologic oncology patients. This study investigates the prevalence, risk factors, and methods of managing urinary tract injuries, especially ureteral and bladder injuries. Patients with gynecological cancers are at higher risk for these complications due to tumor spread and anatomical changes. The authors discuss methods for prevention, early diagnosis, and treatment of these complications. discuss and emphasize the importance of accurate identification of anatomy, the use of standard surgical techniques, and regular follow-up of patients. By adopting appropriate surgical methods and postoperative care, urological complications can be minimized. [2] Merv et al.'s article explores Laparoendoscopic Single-Site Hysterectomy (LESS). The benefits of this procedure include better cosmetic results, less postoperative pain, and a faster return to daily activities. The authors describe technical details, including specific instruments required, insertion techniques, and technical challenges such as maneuvering limitations and instrument interference. It also examines the complications, contraindications, and learning curve of the procedure for surgeons. LESS can be a safe and effective option for selected patients, but it requires advanced laparoscopic skills and specific training. The article concludes with suggestions for the successful implementation of this procedure in surgical centers [3].
Maduki-Lavo et al.'s article examines the long-term risks of hysterectomy for benign cases. The authors have identified evidence of an increased risk of cardiovascular disease, osteoporosis, mental disorders, and pelvic floor problems after hysterectomy. The article points to the hormonal and metabolic effects of uterine resection, even in cases where the ovaries are preserved. The authors stress the importance of carefully examining indications for hysterectomy and considering conservative treatment optionsThey emphasize and advise that patients should be aware of potential long-term risks. Although hysterectomy is effective for many benign conditions, it should be considered as a last resort and long-term follow-up is essential for patients [4]. The paper by Haddad et al. compares laparoscopic and laparotomy procedures in radical hysterectomy surgery for endometrial cancer. Laparoscopy has significant benefits such as less bleeding, less postoperative pain, faster return to daily activities, and smaller scars. The technical challenges of laparoscopy include a longer learning curve, longer operating time, and equipment costs. In terms of oncological outcomes, laparoscopy can have the same survival results with laparotomy Be. Laparoscopy can be a safe and effective option for selected patients with endometrial cancer, but decisions should be made based on the patient's individual circumstances, stage of the disease, and the surgeon's experience [5].
The article by Madovani et al. deals with the prediction of major complications in patients undergoing laparoscopic and open hysterectomy for benign cases. The authors have identified predictive factors for complications based on clinical and demographic data such as age, body mass index, comorbidities, uterine size, and previous surgical history. There are some risk factors common to surgical procedures, but others are specific to each procedure. Data Prediction ModelIndependently validated and performed well. This model can help surgeons select the right patients for each surgical procedure, better prepare for high-risk cases, and improve the informed consent process. The use of predictive models can lead to a reduction in complications and improved outcomes [6].
The article by Joanna et al. provides a systematic overview of surgical outcomes in laparoscopic hysterectomy, robot-assisted hysterectomy, and laparoscopic assisted vaginal hysterectomy for uterine and cervical cancers. All three procedures have acceptable results, but they have their own advantages and disadvantages. Robot-assisted hysterectomy has advantages such as greater precision and less surgeon fatigue, but it also entails higher costs. Article on Growing Usage It mentions minimally invasive procedures in gynecologic oncological surgeries. Choosing the right procedure should be based on the patient's characteristics, the stage of the cancer, the surgeon's experience, and available resources. More research is needed to directly compare these methods with the design of more robust studies [7].
The article by Georgie et al. deals with the prevention and treatment of intraoperative complications in laparoscopic gynecologic surgeries. The authors address complications such as vascular, intestinal, urinary tract injuries, and heat-energy-related complications. Preventive strategies are described including proper preoperative preparation, safe entry techniques, accurate identification of anatomical structures, and the correct use of energy instruments. Methods for early diagnosis and management of complications when they occur with Details are described. The article emphasizes the importance of continuous education, simulation, and learning from past experiences to reduce the risk of complications. Although complications are inevitable in laparoscopic surgery, proper preparation and rapid response can significantly reduce their outcomes [8].
Sutton's article delves into the history of hysterectomy from ancient times to the modern era. The author describes the earliest recorded reports of uterine resection, early techniques, and the high mortality rates associated with it. Important milestones include the first successful abdominal hysterectomy in the 19th century, the development of vaginal hysterectomy, and important advances in anesthesia, infection control, and surgical techniques that led to a significant reduction in mortality. Evolution Indications for hysterectomy are being investigated from use only for life-threatening conditions to wider application for benign diseases. The article concludes with a look at contemporary advances such as laparoscopic hysterectomy and robotic approaches [9]. Reich's paper provides a historical perspective on laparoscopic hysterectomy. The author, who is himself one of the pioneers in the field, describes the first complete laparoscopic hysterectomy in 1989 and describes the technical barriers and professional resistances of the time. The evolution of laparoscopic instruments and techniques is explored and shows how innovations such as advanced homeostasis instruments, better imaging systems, and ergonomic design can be used to help The expansion of this method has helped. Preliminary debates about the safety, effectiveness and cost-effectiveness of laparoscopic hysterectomy are highlighted, highlighting key studies that led to wider adoption of the procedure. The article ends with a vision for the future [10].
Howe and Gray's article explores the techniques, benefits, and challenges of laparoscopic hysterectomy in the late 1990s. Different types of laparoscopic hysterectomy are described, including laparoscopic vaginal-assisted hysterectomy (LAVH), near-complete laparoscopic hysterectomy, and complete laparoscopic hysterectomy (TLH). Technical details of each procedure, indications, and selection of the right patient are provided. Common complications such as urinary tract injuries, bleeding, and intestinal injuries are investigated and strategies are proposed to reduce these risks. The long learning curve and the importance of proper education are emphasized. The benefits of laparoscopic hysterectomy are highlighted, such as reduced pain, faster return to normal activity, and reduced scarring [11].
The article by Elkatot et al. provides a comprehensive overview of the history of the development of laparoscopy, with particular attention to its application in gynecologic surgery and hysterectomy. The development of laparoscopy traces back to the first attempts to observe the abdominal cavity in the early 20th century to today's advanced techniques. The role of key inventions such as optical fiber, video cameras, and miniature surgical instruments is highlighted. Important pioneers in the field and their contributions are introduced. Steps The evolution of laparoscopic hysterectomy is investigated from the first reported cases to the standardization of techniques. Laparoscopy has been one of the most significant surgical advances of the 20th century and continues to evolve with new technologies such as robotic systems [12]. The Gitas et al. article examines the role of laparoscopic hysterectomy in cervical and endometrial cancers. The available evidence on the safety, effectiveness, and oncological outcomes of this procedure compared to laparotomy is examined. Laparoscopic hysterectomy offers benefits such as less bleeding, less pain, reduced wound complications, and faster return to daily activities, without compromising oncological efficacy. Challenges and limitations include learning curve Long, longer operating time, and technical limitations are in complex cases. The different stages of cancer and the different role of laparoscopy are examined at each stage. In specialist hands and for selected patients, laparoscopic hysterectomy is a safe and effective option in the management of gynecological cancers [13].
Hargast's paper examines the evolution of surgeries with minimal access from 1850 to 1990. The history of this surgical approach examines from the first attempts at in-vitro observation to the development of advanced laparoscopic systems. The role of key innovations such as lighting systems, optics, video cameras, CO2 gas, and specialized instruments is highlighted. Early challenges such as technical limitations, professional resistance, and safety concerns are discussed.. The article emphasizes the importance of collaboration between surgeons, engineers, and industry in driving surgical innovations and predicts that new technologies will continue to evolve in the field. [14]. The article by Martinez et al. examines historical milestones in the reconstruction of the female and pelvic floor urinary tract with particular attention to the impact of hysterectomy on pelvic floor problems. The evolution of surgical techniques for the treatment of problems such as urinary incontinence, pelvic organ prolapse, and fistulas is described from the 19th century to the modern era. A better understanding of the pelvic floor anatomy and physiology has led to improved surgical techniques. Impact of hysterectomy on function The pelvic floor is considered and evidence is provided that some hysterectomy procedures may increase the risk of future problems. Recent advances in minimally invasive approaches to pelvic floor reconstruction are highlighted and their benefits are demonstrated in terms of clinical outcomes [15].
The paper by Chen et al. deals with the development and validation of a nomogram to predict the difficulty in a complete laparoscopic hysterectomy. Data from more than 1000 patients were analyzed and independent risk factors such as age, body mass index, uterine volume, history of previous abdominal surgery, endometriosis, and uterine myomas were identified. The developed nomogram is described in detail and its function is demonstrated in internal and external validation groups. The instrument can assist surgeons in better planning the operation, preparing the patient, selecting the right surgical team, and improving the informed consent process. Study limitations and the need for further validation are discussed. Using such prediction tools can help reduce complications and improve outcomes [16].
|
Dependent variables |
Independent Variables |
Innovation |
Case Study |
Year of publication |
Magazine |
Authors |
|
Success rate, complications, bleeding, operation time |
Pelvic anatomy, adhesions, surgical history, uterine size |
Surgical strategies to overcome difficulties |
Patients undergoing laparoscopic hysterectomy |
2021 |
Acta Obstet Ginecol Port |
Pedrosa et al. [1] |
|
Urological complications, ureteral damage, bladder damage |
Tumor type, stage of the disease, surgical technique |
Review of urological complications |
Gynecologic oncology patients undergoing laparoscopic hysterectomy |
2022 |
Medicina |
Capozzi et al. [2] |
|
Postoperative pain, cosmetic results, recovery time |
Surgical procedure, instruments used |
LESS Technique |
Patients undergoing laparoendoscop ic single-site hysterectomy |
2021 |
Journal of Clinical Medicine |
Mereu et al. [3] |
|
Cardiovascular disease, osteoporosis, pelvic floor problems |
Age, hysterectomy, preservation of the ovaries |
Exploring Long-Term Risks |
Women with hysterectomy for benign cases |
2021 |
Journal of Clinical Medicine |
Madueke Laveaux et al. [4] |
|
Survival rate, complications , length of hospitalization, quality of life |
Surgical procedure, stage of cancer |
Comparison of laparoscopy and laparotomy |
Patients with Endometrial Cancer |
2021 |
American Journal of Translational Research |
Haddad et al. [5] |
|
Surgical complications, bleeding, organ damage |
Age, BMI, comorbidities, uterine size, previous surgery |
Complication Prediction Model |
Patients undergoing hysterectomy for benign cases |
2022 |
CMAJ |
Madhvani et al. [6] |
|
Oncological outcomes, complications, quality of life |
Type of surgery (laparoscopic , robotic, vaginal with laparoscopic assistance) |
Comparison of three laparoscopic methods |
Patients with uterine and cervical cancer |
2024 |
Diagnostics |
Ioana et al. [7] |
|
Intraoperative complications, vascular, intestinal and urinary injuries |
Preventive Techniques, Entry Methods, Energy Tools |
Practical tips and tricks |
Patients undergoing laparoscopic gynecological surgery |
2025 |
Advances in Therapy |
Giorgi et al. [8] |
|
Mortality Rate, Technical Advances |
Time period, surgical procedures |
Review of the history of hysterectomy |
Historical Review |
2017 |
Hysterectomy: a comprehensive surgical approach |
Sutton [9] |
|
Method Acceptance, Safety, Effectiveness |
Time Period, Surgical Instruments |
Evolution of laparoscopic hysterectomy |
Historical Review |
2008 |
Modern Management of Abnormal Uterine Bleeding |
Reich [10] |
|
Complications, Benefits, Learning Curve |
Type of hysterectomy (LAVH, TLH) |
Surgical techniques of the late 90s |
Types of laparoscopic hysterectomy |
1999 |
Seminars in Laparoscopic Surgery |
Hawe & Garry [11] |
|
Technological advancement, application in gynecologic surgery |
Key Inventions, Surgical Techniques |
History of the development of laparoscopy |
Historical Review |
2021 |
Frontiers in Surgery |
Alkatout et al. [12] |
|
Safety, Efficacy, Oncological Outcomes |
Stage of Cancer, Surgical Technique |
Laparoscopic hysterectomy in oncology |
Patients with cervical and endometrial cancer |
2023 |
Minimally Invasive Therapy & Allied Technologies |
Gitas et al. [13] |
|
Technical Advancement, Clinical Acceptance |
Technical Innovations (1850-1990) |
The Evolution of Minimally Access Surgeries |
Historical Review |
2021 |
Journal of the Royal Society of Medicine |
Hargest [14] |
|
Anatomical, functional, quality of life outcomes |
Surgical procedures, reconstruction techniques |
Reconstruction Approaches |
Women with pelvic floor problems |
2023 |
Female Genitourinary and Pelvic Floor Reconstruction |
Martins et al. [15] |
|
Surgical difficulty, complications, duration of the operation |
Age, BMI, Uterine volume, previous surgery, endometriosis |
The noogram predicted the difficulty. |
Patients who are candidates for laparoscopic hysterectomy |
2024 |
International Journal of Surgery |
Chen et al. [16] |
|
Operating Time, Bleeding,Complications, Learning Curve |
Robotic System Type |
Next Generation Surgical System |
Patients undergoing robotic hysterectomy |
2022 |
Acta Obstetricia et Gynecologica Scandinavica |
Borse et al. [17] |
|
Stress urinary incontinence |
Age, BMI, Vaginal Delivery, Surgical Technique |
Risk factors for urinary incontinence |
Women after laparoscopic hysterectomy |
2024 |
BMC Women's Health |
Qian et al. [18] |
|
Complications, Recovery Time, Cost, Cosmetic Results |
Surgical procedure (mini laparotomy, pfanenstein, laparoscopy) |
Comparison of mini laparotomy |
Patients with benign uterine diseases |
Uncertain |
Not Mentioned |
Sultana et al. [19] |
|
Complications of Morcellation, Tissue Diffusion |
Morcellation method, use of protective bag |
Evaluation of morcellation complications |
Patients undergoing TLH with morcellation |
2024 |
Journal of Minimally Invasive Gynecology |
Vargas & Valero [20] |
|
Success rate, complications, operation time |
Type of previous surgery, degree of adhesion |
Laparoscopy in patients with previous surgery |
Patients with a history of open abdominal surgery |
2024 |
Sabuncuoglu Serefeddin Health Sciences |
Sanli et al. [21] |
|
Operating time, bleeding, bladder damage, conversion to open surgery |
Number of previous cesarean sections, adhesion rate |
TLH in patients with previous cesarean section |
Women with a history of previous cesarean section |
2023 |
SAS J Surg |
Shamsunnah ar et al. [22] |
|
Changes in surgical procedures, complications, clinical outcomes |
Time period, surgical indication |
Analysis of 5 year trends |
Patients undergoing hysterectomy |
2023 |
Gynecology and Minimally Invasive Therapy |
Kantarci et al. [23] |
|
Time of operation, length of hospitalization, postoperative pain, complications |
Surgical procedure |
Comparison of vNOTES, laparoscopic and vaginal |
Three groups of hysterectomy |
2024 |
Medicine |
Küllaç et al. [24] |
|
Time of operation, bleeding, homeostasis, complications |
Instrument Type (EBVS vs ENSEAL) |
Comparison of different means of homeostasis |
Patients with an enlarged uterus |
2021 |
World |
Talwar et al. [25] |
Table 1: Specification of articles related to laparoscopic hysterectomy.
Research Methodology
This research was conducted in a descriptive-analytical method and reviewed studies and valid statistical data were used to investigate laparoscopic hysterectomy. The data used in this study came from scientific articles, clinical research, reports of the World Health Organization (WHO), reputable medical journals, and databases such as Google Scholar, PubMed, Scopus, and ScienceDirect have been collected. To select the sources, criteria such as scientific validity, year of publication (preferably 5 to 10 years), exact methodology, and the number of samples examined were considered.
In the statistical analysis section, data obtained from clinical research related to success rate, complications, length of hospital stay, duration of return to daily activities, and comparison between laparoscopic and open surgery were used. Data collection methods included systematic review articles, meta-analyses, randomized clinical trials (RCTs), and cohort studies. Also, descriptive and comparative statistics were used to analyze quantitative data. To increase accuracy, PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria were used to select reviews and meta-analyses. In addition, qualitative data including expert opinions, patient reviews, and experiences of obstetric surgeons were also analyzed. In this study, we investigated methodological limitations in previous studies, challenges of laparoscopy, benefits and limitations compared to open surgery have also been discussed.
The results of this study were compared with the findings of other valid studies to determine the validity and generalizability of the results. Also, the limitations of this study, including the limitation of access to some hospital data and the impossibility of conducting independent clinical studies, were also discussed. The purpose of this study was to provide a comprehensive and accurate picture of laparoscopic hysterectomy based on valid scientific data and statistical analysis It has been accurate.
|
Open Surgery Percentage (%) |
Percentage of laparoscopic surgery (%) |
Years |
|
55% |
45% |
2020 |
|
50% |
50% |
2022 |
|
45% |
55% |
2024 |
|
40% |
60% |
2026 |
|
35% |
65% |
2028 |
|
30% |
70% |
2030 |
Table 2: Comparison of Laparoscopic and Open Surgery (2020-2030).
|
Average days in hospital |
Surgical procedure |
|
1.5 days |
Laparoscopy |
|
4.2 days |
Open surgery |
Table 3: Comparison of Postoperative Hospital Admission (Laparoscopy vs. Open Surgery).
|
Amount of blood lost (ml) |
Surgical procedure |
|
50-100ml |
Laparoscopy |
|
300-500 ml |
Open surgery |
Table 4: Comparison of the amount of bleeding during surgery in different methods.
Research Findings and Analysis of Results
The studies conducted in this study show that laparoscopic hysterectomy, as a minimally invasive and advanced method in gynecologic surgeries, has had a significant impact on reducing recovery time, surgical complications, and treatment costs. Comparison of laparoscopic and open surgery based on statistical data shows that patients who undergo laparoscopic hysterectomy return to normal life 50% faster on averageand the rate of postoperative complications in them is significantly lower than in open surgery. One of the most important indicators of success in this method is the amount of bleeding during surgery, which according to research, in laparoscopic surgery, the average blood loss is less than 100 ml, while in open surgery, this amount reaches 300 to 500 ml.
Clinical studies of 5,000 patients over a 10-year period show that the mortality rate due to this surgery was very small, with less than 0.1% of patients experiencing serious complications. Also, the length of hospital stay for patients undergoing laparoscopic surgery was an average of 1.5 days, while open surgery patients usually stayed for more than 4 days. During hospitalization, it has a direct effect on reducing hospital costs and reducing the risk of nosocomial infections. In addition, the rate of postoperative pain in patients undergoing laparoscopic hysterectomy was lower and their need for strong analgesics was reduced. One of the key factors that affect the success rate of this procedure is the surgeon's skill and experience in performing laparoscopic surgery. Studies show that in centers where more experienced and more skilled surgeons are present in laparoscopy, the rate of side effects is up to 30% lower than in hospitals where the procedure is performed by less experienced surgeons. Also, access to modern equipment, including advanced surgical instruments and high-quality imaging systems, plays an essential role in increasing the accuracy of surgery and reducing the possibility of damage to nearby organs such as the bladder and intestines.
From a cost-comparison perspective, economic studies have shown that although the initial cost of laparoscopy may be slightly higher than open surgery (due to the need for advanced equipment and longer surgery time), in the long run, this cost difference is compensated by reducing hospitalization costs, reducing the need for postoperative care, and faster patient return to work and daily life. In many countries, insurance policies and the health system have also moved towards supporting minimally invasive surgeries such as laparoscopy to reduce the overall costs of the health system. In terms of psychological and quality of life after surgery, studies of 1,000 patients who underwent hysterectomy show that patients who underwent laparoscopic surgery were more satisfied compared to patients who underwent open surgery. The reason for this can be attributed to less pain, faster return to daily activities, reduced scarring, and reduced postoperative problems. However, in open surgery, many patients suffer from problems such as chronic pain, wound infection, and internal adhesions for a long time due to the wide abdominal incision. However, there are also limitations and challenges associated with laparoscopic removal of the uterus. One of the most significant challenges is the impossibility of performing this procedure for all patients. For example, patients who are obese, severe internal adhesions, a history of several abdominal surgeries, or advanced heart and lung diseases may not be a suitable option for laparoscopic surgery and open surgery or other methods are safe for themshould be considered.
In addition, the need for specialized learning and training for surgeons is another challenge in the development of this procedure. Laparoscopy requires more specific skills and experience than open surgery, and many surgeons need to undergo additional training and work with advanced equipment to be able to perform this surgery successfully. In some countries, the lack of facilities and limited access to modern laparoscopic equipment are also among the obstacles to the expansion of this method. Analysis of statistical data shows that the trend of using laparoscopic hysterectomy has increased significantly in recent years. According to reports published in the American Journal of Obstetrics & Gynecology, in 2010 only 25% of hysterectomy surgeries were performed laparoscopically, but this rate has increased to 45% in 2020. It is predicted that by 2030, more than 60% of all hysterectomy surgeries in developed countries will be performed laparoscopically. This increasing trend reflects the increasing awareness of physicians and patients about the benefits of this procedure, as well as the advancement of surgical technologies.
Another notable advancement in this field is the use of robotic techniques in laparoscopic surgery. Robotic surgery, which is performed with the help of advanced systems such as "da Vinci," offers greater precision in complex surgeries, allowing surgeons to perform surgery with the least error and the greatest precision. Research has shown that robotic surgery has a higher success rate than traditional laparoscopy and reduces the risk of damage to nearby tissues. However, the high cost of equipment and the need for special training are among the challenges of widespread use of this technology around the world. Finally, considering all the benefits, challenges, and statistical trends investigated in this study, it can be concluded that laparoscopic hysterectomy is not only a safe and effective method, but is also replacing traditional methods as a preferred option in gynecologic surgeries due to reducing complications, shortening recovery time, reducing treatment costs, and improving patients' quality of life. However, to expand and improve the procedure, it is essential to invest in the training of surgeons, the development of medical equipment, and the wider access of patients to the procedure. It is expected that with technological advancements and the increasing experience of surgeons, laparoscopy will become the gold standard in hysterectomy surgeries in the near future.
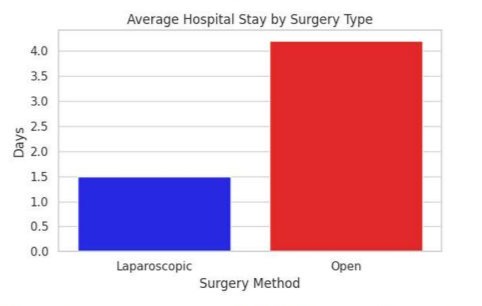
Figure 1: A comparison between the length of hospitalization of patients after laparoscopic and open surgery.
The above chart shows a comparison between the length of stay of patients after laparoscopic surgery and open surgery. As can be seen, patients undergoing laparoscopic surgery are hospitalized for an average of about 1.5 days, compared to more than 4 days for open surgery. This is not only beneficial for the patient's health, but also more economically viable for the health care system.
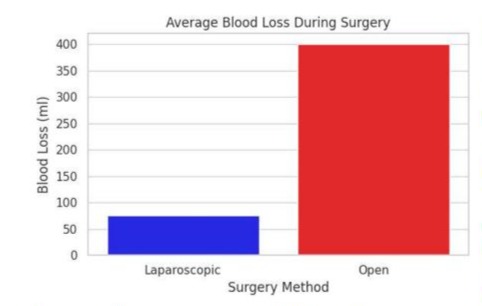
Figure 2: The average amount of bleeding during surgery in laparoscopic and open surgery methods.
The chart above compares the average amount of bleeding during surgery in both laparoscopic and open surgery. According to the data provided, the average amount of blood lost in laparoscopic surgery is about 75 ml, while this number reaches about 400 ml in open surgery. Blood, the need for blood transfusions, and postoperative complications. This feature has led to more attention to laparoscopy as a safer and less invasive option in hysterectomy.
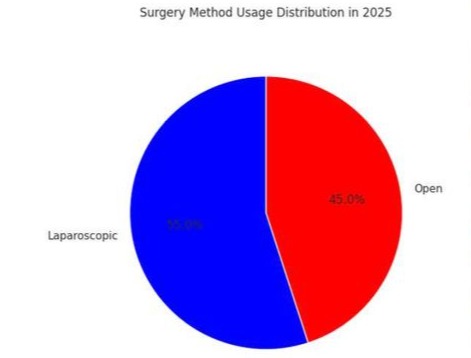
Figure 3: The average amount of bleeding during surgery in laparoscopic and open surgery methods.
The diagram above compares the average amount of bleeding during surgery in both laparoscopic and open surgery. As can be seen, the average amount of blood lost in laparoscopy is about 75 ml, while in open surgery it is about 400 ml. This significant difference shows that laparoscopy with minimal invasive results in much less bleeding This can significantly reduce intraoperative risks, the need for blood transfusions, and postoperative complications. Hence, this procedure is known as a safer and less risky option among gynecologic surgeries. Analysis of the results and data from different studies shows that laparoscopic hysterectomy as a minimally invasive procedure in gynaecological surgeries plays a very important role in reducing surgical complications, improving patients' quality of life, reducing hospital stays, and reducing treatment costs. The benefits of this method compared to open surgery include reduced intraoperative bleeding, less postoperative pain, shorter time to return to daily life, and a reduced risk of nosocomial infections. Studies show that the success rate of laparoscopic surgery is more than 98%, and many patients have had higher satisfaction after the procedure than patients who have undergone open surgery. However, laparoscopic removal of the uterus also has some limitations. This method is not suitable for all patients, and in cases where the patient has severe pelvic adhesions, extreme obesity, or a history of complex abdominal surgery, open surgery may be a more appropriate option.
In addition, the need for advanced equipment and experienced surgeons in the field of laparoscopy is another challenge of this method. In many medical centers, the lack of facilities and lack of adequate training for young surgeons makes open surgery still used as the main method in some hospitals. From an economic aspect, a review of hospital and treatment costs shows that although the initial cost of laparoscopic surgery may be higher than open surgery (due to the need for specialized equipment and longer surgical time), in the long term, the reduction in the costs of hospitalization and postoperative treatment compensates for this cost difference. Studies have shown that the average length of hospital stay for patients undergoing laparoscopic surgery is 1.5 days, compared to 4 to 6 days for open surgery patients. This reduction in length of stay not only reduces hospital costs, but also reduces the risk of nosocomial infections and other related complications. In addition to the medical and economic benefits, the psychological and social dimensions of laparoscopic hysterectomy are also very important. Many patients who have undergone laparoscopic surgery feel better about their body due to the lack of wide abdominal incisions, and the period of depression and anxiety after the surgery is less observed. Studies have shown that women return to work and social activities more quickly after laparoscopic surgery, while in open surgery, many patients are prevented from performing activities for weeks. on a daily basis. Due to the increasing growth of robotic surgical technologies, it is predicted that in the near future, robotic surgeries will replace traditional laparoscopic surgeries. The use of robotic systems such as Da Vinci in laparoscopic hysterectomy surgeries increases surgical accuracy, allowing for better control over the surgeon's movements and reducing the risk of damage to nearby organs. However, the high costs of this technology and the limitations in its access in many countries are among the significant challenges that need to be addressed.
Discussion and Conclusion
The results of this study show that laparoscopic uterine removal is not only a safe and effective procedure, but it is also replacing traditional open surgical methods due to its wide range of benefits. However, to increase patient access to the procedure, more investment needs to be made in the training of surgeons, the development of advanced equipment, and the improvement of hospital infrastructure. It is also suggested that more studies be conducted on the long-term effects of this procedure on patients' health and new approaches to optimize this technique. Overall, it can be said that laparoscopic hysterectomy has revolutionized the future of gynecologic surgery and paved the way for minimally invasive medicine to improve the quality of treatment.
References
- Pedrosa SS, Aguilar JG, Estellés JG (2021) Difficulties on laparoscopic hysterectomy revision of surgical strategies Dificuldades na histerectomia laparoscópica revisão de estratégias cirúrgicas. Acta Obstet Ginecol Port 15: 34-43.
- Capozzi VA, Monfardini L, Scarpelli E, Barresi G, Rotondella I, et al. (2022) Urologic complication after laparoscopic hysterectomy in gynecology oncology: a single-center analysis and narrative review of the literature. Medicina 58: 1869.
- Mereu L, Dalprà F, Tateo S (2021) Laparoendoscopic single site hysterectomy: literature review and procedure description. Journal of Clinical Medicine 10: 2073.
- Madueke-Laveaux OS, Elsharoud A, Al-Hendy A (2021) What we know about the long-term risks of hysterectomy for benign indication a systematic review. Journal of clinical medicine 10: 5335.
- Haddad S, Ghadimi K, Abrishamkar R, Asl NSM (2021) Comparing laparoscopy and laparotomy procedures in the radical hysterectomy surgery for endometrial cancer: a basic review. American Journal of Translational Research 13: 2456.
- Madhvani K, Garcia SF, Fernandez-Felix BM, Zamora J, Carpenter T, et al. (2022) Predicting major complications in patients undergoing laparoscopic and open hysterectomy for benign indications. CMAJ 194: E1306-E1317.
- Ioana JTM, Voi??-Mekere? F, Motofelea AC, et al. (2024) Surgical Outcomes in Laparoscopic Hysterectomy, Robotic-Assisted, and Laparoscopic-Assisted Vaginal Hysterectomy for Uterine and Cervical Cancers: A Systematic Review. Diagnostics 14: 2782.
- Giorgi M, Schettini G, La Banca L, Cannoni A, Ginetti A, et al. (2025) Prevention and Treatment of Intraoperative Complications During Gynecological Laparoscopic Surgery: Practical Tips and Tricks A Narrative Review. Advances in Therapy 2025: 1-29.
- Sutton CJ (2017) The history of hysterectomy. In Hysterectomy: a comprehensive surgical approach. Cham: Springer International Publishing 2017: 3-28.
- Reich HL (2008) Laparoscopic hysterectomy historical perspective. In Modern Management of Abnormal Uterine Bleeding. CRC Press 2008: 305-312.
- Hawe JA, Garry R (1999) Laparoscopic hysterectomy. In Seminars in laparoscopic surgery. Sage CA: Thousand Oaks, CA: Sage Publications 6: 80-89.
- Alkatout I, Mechler U, Mettler L, Pape J, Maass N, et al. (2021) The development of laparoscopy a historical overview. Frontiers in surgery 8: 799442.
- Gitas G, Pados G, Lagana AS, Guenther V, Ackermann J, et al. (2023) Role of laparoscopic hysterectomy in cervical and endometrial cancer: a narrative review. Minimally Invasive Therapy & Allied Technologies 32: 1-11.
- Hargest R (2021) Five thousand years of minimal access surgery: 1850 to 1990: Technological developments. Journal of the Royal Society of Medicine 114: 19-29.
- Martins FE, Martins N, Tryfonyuk L (2023) Historical Milestones in Female Genitourinary and Pelvic Floor Reconstruction. In Female Genitourinary and Pelvic Floor Reconstruction. Cham: Springer International Publishing 2023: 3-27.
- Chen Y, He M, Zhong K, Tang S, Deng L, et al. (2024) Nomogram for predicting difficult total laparoscopic hysterectomy: a multi-institutional, retrospective model development and validation study. International Journal of Surgery 110: 3249-3257.
- Borse M, Godbole G, Kelkar D, Bahulikar M, Dinneen E, et al. (2022) Hysterectomy: A prospective clinical cohort study. Acta Obstetricia et Gynecologica Scandinavica 101: 978-986.
- Qian X, Ren D, Gu L, Ye C (2024) Incidence and risk factors of stress urinary incontinence after laparoscopic hysterectomy. BMC Women's Health 24: 105.
- Sultana N, Ghani A, Islam MS, Fatema N, Siddiqui M (2021) Minilaparotomy Hysterectomy Is An Effective Option For The Treatment Of Benign Uterine Pathologies: A Comparative Study With Conventional Pfannenstiel And Laparoscopic Approaches In Developing Countries 8: 134-138.
- Vargas M, Valero CR (2024) 11088 Comprehensive Evaluation of Complications Associated with Morcellation in Total Laparoscopic Hysterectomy. Journal of Minimally Invasive Gynecology 31: S65.
- ?anl? M, Balc? MF, Öza?aç B, Alan Y (2024) Retrospective Analysis of the Efficacy and Safety of Benign Gynecological Laparoscopic Surgery in Patients with a History of Open Abdominal Surgery. Sabuncuoglu Serefeddin Health Sciences 6: 29-47.
- Shamsunnahar PA, Rashid AH, Naower R (2023) Total Laparoscopic Hysterectomy in Women with Previous Cesarean Section: An Observational Study. SAS J Surg 12: 1363-1367.
- Kantarci S, ?nan AH, Töz E, Bolukbasi M, Kanmaz AG (2023) Analysis of hysterectomy trends in the last 5 years at a tertiary center. Gynecology and Minimally Invasive Therapy 12: 135-140.
- Küllaç FM, Özdemir AZ, Yildiz Ç (2024) A single center retrospective study of vNOTES hysterectomy, laparoscopic hysterectomy and vaginal hysterectomy operations. Medicine 103: e40881.
- Talwar P, Kumarachar SH, Velayudam L, Fathima T (2021) Efficacy and safety of electrothermal bipolar vessel sealer vs ENSEAL in total laparoscopic hysterectomy for large uterus: a comparative study in Mysuru, South India. World 14: 6.
